Endometrial polyp
| Endometrial polyp | |
|---|---|
| Other names | Uterine polyp |
 | |
| Endometrial polyp, viewed by sonography | |
| Specialty | Gynecology |
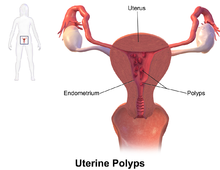
An endometrial polyp or uterine polyp is a mass in the inner lining of the uterus.[1] They may have a large flat base (sessile) or be attached to the uterus by an elongated pedicle (pedunculated).[2][3] Pedunculated polyps are more common than sessile ones.[4] They range in size from a few millimeters to several centimeters.[3] If pedunculated, they can protrude through the cervix into the vagina.[2][5] Small blood vessels may be present, particularly in large polyps.[2]
Signs and symptoms[edit]
They often cause no symptoms.[4] Where they occur, symptoms include irregular menstrual bleeding, bleeding between menstrual periods, excessively heavy menstrual bleeding (menorrhagia), and vaginal bleeding after menopause.[3][6] Bleeding from the blood vessels of the polyp contributes to an increase of blood loss during menstruation and blood "spotting" between menstrual periods, or after menopause.[7] If the polyp protrudes through the cervix into the vagina, pain (dysmenorrhea) may result.[5]
Cause[edit]
No definitive cause of endometrial polyps is known, but they appear to be affected by hormone levels and grow in response to circulating estrogen.[3] Risk factors include obesity, high blood pressure and a history of cervical polyps.[3] Taking tamoxifen or hormone replacement therapy can also increase the risk of uterine polyps.[3][8] The use of an intrauterine system containing levonorgestrel in women taking tamoxifen may reduce the incidence of polyps.[9]
Diagnosis[edit]


Endometrial polyps can be detected by vaginal ultrasound (sonohysterography), hysteroscopy and dilation and curettage.[3] Detection by ultrasonography can be difficult, particularly when there is endometrial hyperplasia (excessive thickening of the endometrium).[2] Larger polyps may be missed by curettage.[10]
Endometrial polyps can be solitary or occur with others.[11] They are round or oval and measure between a few millimeters and several centimeters in diameter.[7][11] They are usually the same red/brown color of the surrounding endometrium although large ones can appear to be a darker red.[7] The polyps consist of dense, fibrous tissue (stroma), blood vessels and glandlike spaces lined with endometrial epithelium.[7] If they are pedunculated, they are attached by a thin stalk (pedicle). If they are sessile, they are connected by a flat base to the uterine wall.[11] Pedunculated polyps are more common than sessile ones.[4]
Treatment[edit]
Polyps can be surgically removed using curettage with or without hysteroscopy.[12] When curettage is performed without hysteroscopy, polyps may be missed. To reduce this risk, the uterus can be first explored using grasping forceps at the beginning of the curettage procedure.[7] Hysteroscopy involves visualising the endometrium (inner lining of the uterus) and polyp with a camera inserted through the cervix. Large polyps can be cut into sections before each section is removed.[7] The presence of cancerous cells may suggest a hysterectomy (surgical removal of the uterus).[3] A hysterectomy is usually not considered when cancer is not present.[7] In either procedure, general anesthetic is typically supplied.[10]
The effects of polyp removal on fertility has not been studied.[13]
Prognosis[edit]
Endometrial polyps are usually benign although some may be precancerous or cancerous.[3] About 0.5% of endometrial polyps contain adenocarcinoma cells.[14] Polyps can increase the risk of miscarriage in women undergoing IVF treatment.[3] If they develop near the fallopian tubes, they may lead to difficulty in becoming pregnant.[3] Although treatments such as hysteroscopy usually cure the polyp concerned, recurrence of endometrial polyps is frequent.[7] Untreated, small polyps may regress on their own.[15]
Epidemiology[edit]
Endometrial polyps usually occur in women in their 40s and 50s.[3] Endometrial polyps occur in up to 10% of women.[2] It is estimated that they are present in 25% of women with abnormal vaginal bleeding.[8]
See also[edit]
References[edit]
- ^ WHO Classification of Tumours Editorial Board, ed. (2020). "6. Tumours of the uterine corpus: Endometrial polyp". Female genital tumours: WHO Classification of Tumours. Vol. 4 (5th ed.). Lyon (France): International Agency for Research on Cancer. p. 268. ISBN 978-92-832-4504-9.
- ^ a b c d e Jane A. Bates (1997). Practical Gynaecological Ultrasound. Cambridge, UK: Cambridge University Press. ISBN 1-900151-51-0.
- ^ a b c d e f g h i j k l "Uterine polyps". MayoClinic.com. 2006-04-27.
- ^ a b c Sternberg, Stephen S.; Stacey E. Mills; Darryl Carter (2004). Sternberg's Diagnostic Surgical Pathology. Lippincott Williams & Wilkins. p. 2460. ISBN 0-7817-4051-7.
- ^ a b Dysmenorrhea: Menstrual abnormalities at Merck Manual of Diagnosis and Therapy Professional Edition
- ^ "Endometrial Polyp". GPnotebook. Retrieved 2007-10-20.
- ^ a b c d e f g h DeCherney, Alan H.; Lauren Nathan (2003). Current Obstetric & Gynecologic Diagnosis & Treatment. McGraw-Hill Professional. p. 703. ISBN 0-8385-1401-4.
- ^ a b Edmonds, D. Keith; Sir John Dewhurst (2006). Dewhurst's Textbook of Obstetrics and Gynaecology. Blackwell Publishing. p. 637. ISBN 1-4051-5667-8.
- ^ Chan SS, Tam WH, Yeo W, et al. (2007). "A randomised controlled trial of prophylactic levonorgestrel intrauterine system in tamoxifen-treated women". BJOG. 114 (12): 1510–5. doi:10.1111/j.1471-0528.2007.01545.x. PMID 17995495. S2CID 21145823.
- ^ a b Macnair, Trisha. "Ask the doctor – Uterine polyps". BBC Health. Retrieved 2007-10-21.
- ^ a b c Bajo Arenas, José M.; Asim Kurjak (2005). Donald School Textbook Of Transvaginal Sonography. Taylor & Francis. p. 502. ISBN 1-84214-331-X.
- ^ "Uterine bleeding – Signs and Symptoms". UCSF Medical Center. 2007-05-08. Archived from the original on 2008-04-11. Retrieved 2007-10-20.
- ^ Jayaprakasan, K; Polanski, L; Sahu, B; Thornton, JG; Raine-Fenning, N (Aug 30, 2014). "Surgical intervention versus expectant management for endometrial polyps in subfertile women" (PDF). The Cochrane Database of Systematic Reviews. 8 (8): CD009592. doi:10.1002/14651858.CD009592.pub2. PMC 6544777. PMID 25172985. Archived from the original (PDF) on November 4, 2018. Retrieved November 4, 2018.
- ^ Rubin, Raphael; David S Strayer (2007). Rubin's Pathology: Clinicopathologic Foundations of Medicine. Lippincott Williams & Wilkins. p. 806. ISBN 978-0-7817-9516-6.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Kaunitz, Andrew M. (2002-08-26). "Asymptomatic Endometrial Polyps: What Is the Likelihood of Cancer?". Medscape Ob/Gyn & Women's Health. Retrieved 2008-04-20.
